Anterior cruciate ligament tears are all too common an injury among athletes. In my practice I see a higher number of female athletes with this injury.
I’m often asked the question “why does it seem girls have this injury more than boys?”
We know from various studies, females can be 3x more likely than their male counterparts to suffer an ACL tear in the same sport. Why is that? Is there any way to reduce this risk?
There are multiple factors associated with this increased risk of ACL tears in female athletes. Their hormonal differences from males as well as fluctuations in the menstrual cycle have been implicated. There are also structural differences in anatomy that account for a greater risk of injury. This includes leg alignment and bone morphology around the ACL. Differences in strength and muscle imbalances can lead to a higher rate of tears. Lastly, and perhaps the one difference that we may have the most control over is what the physical therapy literature refers to as ” dynamic valgus collapse”.

This term refers to the position that a female athlete’s knee gets into many times during athletic performance. The knee gets flexed inward with the femur (thigh bone) rotated inward and the tibia (leg bone) rotated outward. Exaggeration of this force across the knee has been shown to be a mechanism by which the ACL gets torn.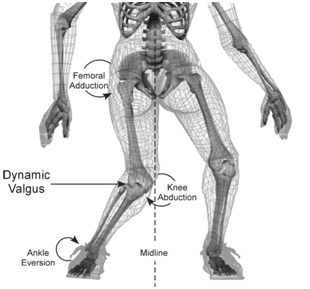
A prevention program including strengthening with plyometrics (emphasis on muscle balance) and educational reinforcement; reminding the athlete to avoid this position, has been shown to decrease the risk. This type of program is highly recommended in high risk sports such as basketball and soccer.
There is no doubt that female athletes are at higher risk for ACL tears than the male athlete. Certainly great strides have been made in attempting to understand this phenomenon as well as in prevention. We must continue to advance our knowledge in these areas so that we continue to decrease the injury rates and keep our athletes safe and “in the game”.
For more information on the diagnosis and treatment of an ACL injury, visist the SportsMED website. We have several videos online you may want to view.

 February 7th, 2014
February 7th, 2014  Suzie Sanders
Suzie Sanders 

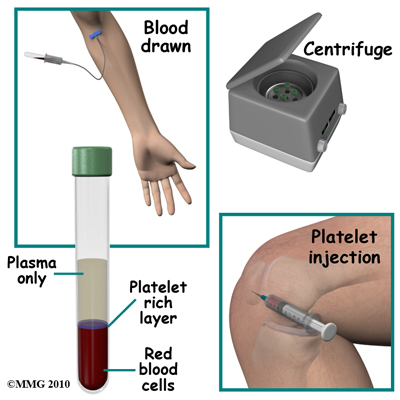 Platelet Rich Plasma (PRP) is one such treatment receiving alot of attention. It is being used for the treatment of a variety of musculoskeletal injuries and conditions. In addition, it is being used to enhance healing of damaged tissues. With reports of athletes like Tiger Woods and Hines Ward turning to this treatment, PRP is becoming a common topic both inside and outside of Orthopedic offices.
Platelet Rich Plasma (PRP) is one such treatment receiving alot of attention. It is being used for the treatment of a variety of musculoskeletal injuries and conditions. In addition, it is being used to enhance healing of damaged tissues. With reports of athletes like Tiger Woods and Hines Ward turning to this treatment, PRP is becoming a common topic both inside and outside of Orthopedic offices.